Can People Recover From COVID- 19 Disease?
by Premier Hospitals | July 1, 2020 |
Imagine If you or someone you know has been infected with the coronavirus, the thought itself is unwelcomed and terrible too. But everybody should know about this situation as it became pandemic. Be aware of yourself what it's to have COVID-19 and recover from it.
Do you feel cold, sneezing, cough, throat pain and breathlessness? Do you feel you are intense and fighting for your life? Eighty-five per cent of infected patients don't need to be hospitalized. They need to be monitored and given medical care. People with the COVID-19 virus can take supportive steps to reduce their symptoms while the body is working to recover from a viral infection.
Symptoms of COVID-19 can appear 5 to 14 days after exposure to the virus. Most people will recover in one or two weeks. In more severe cases, recovery may take six weeks or more. While most patients recover, some experience lung scars and other health conditions. They may also experience weakness, loss of muscle mass, stress, anxiety, and general memory changes. When these conditions are identified, there are management approaches that can help improve these conditions and improve the quality of life of patients and families.
Let us go through this article provided by Premier Hospital gives information about COVID-19 recovery.
Recovery from COVID-19
 The recovery process of COVID-19, including the speed at which you can expect recovery, depends on whether you have a mild, moderate, or severe disease.
Mild disease - 80% and more suffer from mild COVID-19: Recovery time: about two
Weeks
The recovery process of COVID-19, including the speed at which you can expect recovery, depends on whether you have a mild, moderate, or severe disease.
Mild disease - 80% and more suffer from mild COVID-19: Recovery time: about two
Weeks
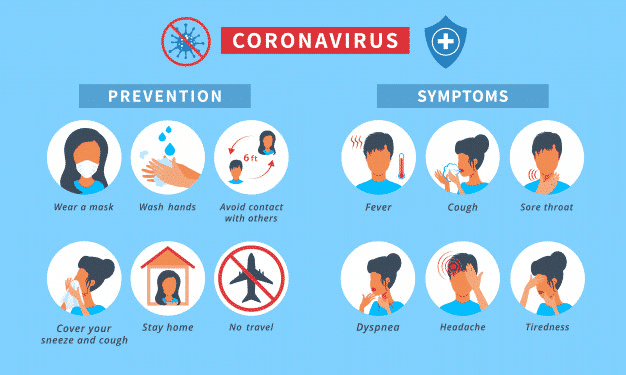
 Symptoms: Many people who are infected with coronavirus have no symptoms and will not know that if not tested. Some have upper respiratory tract infections, fever, cough, and other mild symptoms such as headaches or conjunctivitis. You may have mild pneumonia. Most people feel they have a slight cold or other viral infection, feel tired. Recovery includes treating symptoms at home, resting and isolation from others. It takes two to fourteen 14 days for the symptoms to appear after exposure to the virus.
Loss of smell or taste is also good evidence that you have COVID and that there are no other flu viruses.
Some patients, especially those who are younger and do not have many or no basic medical conditions, may feel unwell for several days or up to a week before they begin to improve. But even if you have mild symptoms and feel normal quickly, doctors recommend that you remain isolated, do not return to public places, or work at least 14 days after symptoms appear and remain fever-free without symptoms. Take medication for three days.
Your recovery from COVID-19 is confirmed when:
Symptoms: Many people who are infected with coronavirus have no symptoms and will not know that if not tested. Some have upper respiratory tract infections, fever, cough, and other mild symptoms such as headaches or conjunctivitis. You may have mild pneumonia. Most people feel they have a slight cold or other viral infection, feel tired. Recovery includes treating symptoms at home, resting and isolation from others. It takes two to fourteen 14 days for the symptoms to appear after exposure to the virus.
Loss of smell or taste is also good evidence that you have COVID and that there are no other flu viruses.
Some patients, especially those who are younger and do not have many or no basic medical conditions, may feel unwell for several days or up to a week before they begin to improve. But even if you have mild symptoms and feel normal quickly, doctors recommend that you remain isolated, do not return to public places, or work at least 14 days after symptoms appear and remain fever-free without symptoms. Take medication for three days.
Your recovery from COVID-19 is confirmed when:
- You are free from fever without using antipyretic drugs for three full days (72 hours).
- Symptoms of coughing and shortness of breath reduce
- It's been seven days since your symptoms began
 Symptoms: The recovery process is longer in people with more acute or anxious COVID-19 symptoms and requires an EP visit or even hospitalization.
Patients with moderate symptoms tend to have more respiratory problems and fever. Many of them describe night fever and sweating and have a strong cough. They can also have difficulty breathing or a feeling of chest pressure or heaviness. It takes a lot of effort to get up and get a glass of water.
Serious diseases can cause pneumonia. About 50% experience shortness of breath and low oxygen levels due to shortness of breath. Most patients experience fever, feel very tired, and dry cough.
Some of these patients will recover at home, but this can take longer than milder cases. To recover, stay in the hospital for several days. Hospital treatment may include oxygen. You will have heart inflammation, chest pain and exercise intolerance can occur. Complete recovery can take about a month or more, and WHO recommends isolation at home at least two weeks after symptoms disappear. People will feel very sick for a few weeks, and it might take a while for their strength and stamina to return.
The critical moment for people with COVID-19 is between six and ten days (since the onset of symptoms). At this point, some start to get better, while others who feel bad continue to feel just as bad. Others can quickly improve in a few days, but then their condition worsens. That's why patients should be monitored for at least ten days, even if you have recovered enough.
Recovery from a severe illness COVID-19: 5% or less have critical diseases related to COVID-19 that require intensive care
Symptoms: The recovery process is longer in people with more acute or anxious COVID-19 symptoms and requires an EP visit or even hospitalization.
Patients with moderate symptoms tend to have more respiratory problems and fever. Many of them describe night fever and sweating and have a strong cough. They can also have difficulty breathing or a feeling of chest pressure or heaviness. It takes a lot of effort to get up and get a glass of water.
Serious diseases can cause pneumonia. About 50% experience shortness of breath and low oxygen levels due to shortness of breath. Most patients experience fever, feel very tired, and dry cough.
Some of these patients will recover at home, but this can take longer than milder cases. To recover, stay in the hospital for several days. Hospital treatment may include oxygen. You will have heart inflammation, chest pain and exercise intolerance can occur. Complete recovery can take about a month or more, and WHO recommends isolation at home at least two weeks after symptoms disappear. People will feel very sick for a few weeks, and it might take a while for their strength and stamina to return.
The critical moment for people with COVID-19 is between six and ten days (since the onset of symptoms). At this point, some start to get better, while others who feel bad continue to feel just as bad. Others can quickly improve in a few days, but then their condition worsens. That's why patients should be monitored for at least ten days, even if you have recovered enough.
Recovery from a severe illness COVID-19: 5% or less have critical diseases related to COVID-19 that require intensive care
 Symptoms: The main reason people with COVID-19 need to be hospitalized is respiratory problems due to low oxygen levels. Severe COVID-19 and pneumonia can cause critical illness, including acute respiratory distress syndrome (ARDS), heart disease, organ dysfunction, and shock. Mechanical ventilators or other modern therapies such as extracorporeal oxygenation devices (heart/lungs) are needed to run the organs while the body is fighting the virus. The risk of death is higher in this situation.
Severely ill patients often have other risk factors, including obesity, diabetes, heart or lung disease, cancer, other immune problems, or over 65 years of age.
This disease becomes more severe in some people when pneumonia develops, or the immune system triggers a powerful "cytokine storm" to get rid of the virus. This strong inflammatory reaction causes what is called acute respiratory distress syndrome (ARDS), which causes lung tissue damage and maybe even respiratory failure. These patients may be in intensive care units, who need more oxygen and may be ventilated. Most patients may have other problems. When a patient is seriously ill, their other organs can shut down.
It can take weeks or months for you to recover from a severe COVID-19 disease. You might be in an intensive care unit and might even use a ventilator. If you recover from a severe case of COVID-19, it may take time for your lung strength and function to return to normal. If you were put on a ventilator, it would take time for you to regain your independence when you get home - and it depends on how much strength or energy you have lost and how much damage occurred to your lungs.
Most patients with COVID-19 don't need a ventilator, and most people don't end up in the intensive care unit. Instead, most of them can be treated on the and oxygen is supplied through the tube into their nostrils. These patients may have breathing problems, especially during exertion, but generally do well with oxygen. They are alert and often talk to their families.
The above is the recovery from COVID-19.
Life after recovery
Symptoms: The main reason people with COVID-19 need to be hospitalized is respiratory problems due to low oxygen levels. Severe COVID-19 and pneumonia can cause critical illness, including acute respiratory distress syndrome (ARDS), heart disease, organ dysfunction, and shock. Mechanical ventilators or other modern therapies such as extracorporeal oxygenation devices (heart/lungs) are needed to run the organs while the body is fighting the virus. The risk of death is higher in this situation.
Severely ill patients often have other risk factors, including obesity, diabetes, heart or lung disease, cancer, other immune problems, or over 65 years of age.
This disease becomes more severe in some people when pneumonia develops, or the immune system triggers a powerful "cytokine storm" to get rid of the virus. This strong inflammatory reaction causes what is called acute respiratory distress syndrome (ARDS), which causes lung tissue damage and maybe even respiratory failure. These patients may be in intensive care units, who need more oxygen and may be ventilated. Most patients may have other problems. When a patient is seriously ill, their other organs can shut down.
It can take weeks or months for you to recover from a severe COVID-19 disease. You might be in an intensive care unit and might even use a ventilator. If you recover from a severe case of COVID-19, it may take time for your lung strength and function to return to normal. If you were put on a ventilator, it would take time for you to regain your independence when you get home - and it depends on how much strength or energy you have lost and how much damage occurred to your lungs.
Most patients with COVID-19 don't need a ventilator, and most people don't end up in the intensive care unit. Instead, most of them can be treated on the and oxygen is supplied through the tube into their nostrils. These patients may have breathing problems, especially during exertion, but generally do well with oxygen. They are alert and often talk to their families.
The above is the recovery from COVID-19.
Life after recovery
 Lack of energy, shortness of breath and loss of appetite were reported by people who recovered from COVID-19. Because of damage to the lungs and other organs caused by viruses, the body needs time to recover and return to its original state. Meanwhile, these people may need to pay attention to their immunity and maintain social distance, because there is a possibility of remission of viral diseases.
Conclusion:
Given the spectrum of disease severity, recovery can vary greatly. Patients with mild symptoms usually return to healthy life quickly. Patients should be aware of how they feel and listen to their bodies, and not just go out and do whatever you usually want to do. There may be some long-term effects, including a lack of energy.
Recovery of hospitalized patients is usually different, much depending on the health of the patient before hospitalization. Sometimes people with heart disease or severe diabetes can recover well after four or six days in the hospital.
To avoid loss of physical function, if possible, get out of bed and sit in a chair and do leg exercises. If people go to the hospital and spend too much time sitting or lying in bed, they have more difficulty functioning when they return.
About 30 to 40% of patients continue to experience health problems after being discharged from the hospital. The best strategy, of course, is to completely prevent COVID-19 infection. Therefore, doctors encourage people to continue to practice keeping a social distance to avoid exposure. However, if you think you are infected, doctors of Premier Hospital suggest you get tested as soon as possible and, if the results are positive, to consult with your doctor.
In general, most patients can be treated outside the hospital. But if you are sick, early treatment can prevent complications. If you have to be hospitalized, it does not mean that you are sick. Only a few patients end up on the ICU. For more information contact Premier Hospital at 077020 01163
Lack of energy, shortness of breath and loss of appetite were reported by people who recovered from COVID-19. Because of damage to the lungs and other organs caused by viruses, the body needs time to recover and return to its original state. Meanwhile, these people may need to pay attention to their immunity and maintain social distance, because there is a possibility of remission of viral diseases.
Conclusion:
Given the spectrum of disease severity, recovery can vary greatly. Patients with mild symptoms usually return to healthy life quickly. Patients should be aware of how they feel and listen to their bodies, and not just go out and do whatever you usually want to do. There may be some long-term effects, including a lack of energy.
Recovery of hospitalized patients is usually different, much depending on the health of the patient before hospitalization. Sometimes people with heart disease or severe diabetes can recover well after four or six days in the hospital.
To avoid loss of physical function, if possible, get out of bed and sit in a chair and do leg exercises. If people go to the hospital and spend too much time sitting or lying in bed, they have more difficulty functioning when they return.
About 30 to 40% of patients continue to experience health problems after being discharged from the hospital. The best strategy, of course, is to completely prevent COVID-19 infection. Therefore, doctors encourage people to continue to practice keeping a social distance to avoid exposure. However, if you think you are infected, doctors of Premier Hospital suggest you get tested as soon as possible and, if the results are positive, to consult with your doctor.
In general, most patients can be treated outside the hospital. But if you are sick, early treatment can prevent complications. If you have to be hospitalized, it does not mean that you are sick. Only a few patients end up on the ICU. For more information contact Premier Hospital at 077020 01163